Positive Expiratory Pressure therapy
Mask PEP video, Pari PEP Video, Thera PEP Video
Positive expiratory pressure (PEP) therapy involves breathing with a slightly active expiration against an expiratory resistance. It is used for:
clearance of excess secretions from the lungs
reducing gas trapping and improving ventilation of the lungs
PEP therapy may be applied through:
- Face mask (close-fitting) with a one-way valve to which expiratory resistors are attached (Fig. 1) or the Pari PEP system 1 device (Fig. 2).

Fig. 1 PARI mask set

2.Mouthpiece with holes of varying diameters, or dial, to apply expiratory resistance (Fig. 3)


PARI PEP S

Fig. 3 Mouthpiece PEP devices
PEP therapy consists of cycles of breathing through a mask or a mouthpiece device, followed by the forced expiration technique and coughing. For low pressure PEP therapy, an optimal pressure is 10 to 20cmH20 during mid-expiration.
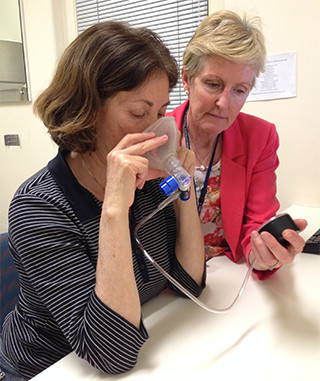
During initial instruction in the technique, a manometer can be placed in parallel with the resistor to determine the expiratory pressure generated and allow adjustments to the breathing technique (Figs 5, 6 & 7).
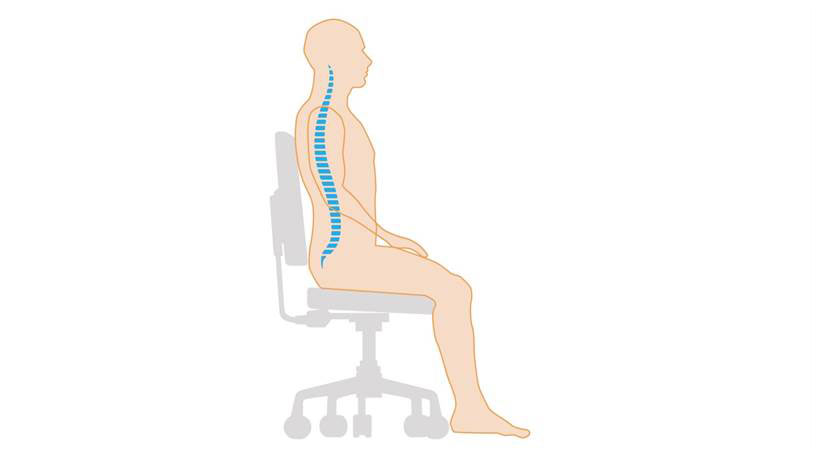
When this technique is taught in the sitting position, the importance of the correct posture should be explained to the patient.
Instruct them to sit in a well-supported chair with a neutral lumbar spine. This enhances the function of the diaphragm and the pelvic floor and minimises musculoskeletal stress (Fig. 4)
The resistance for PEP is selected according to the coloured resistors which are positioned on the white expiratory valve attached to the PEP mask or the hole-sizes of a PARI PEP device if it is used with a mask.
Select the optimal resistor to achieve an expiratory pressure of 10 to 20cmH20 with the least effort for the patient. Hole-sizes commonly chosen during the teaching session are 2.5 and 3.0 (see “Selecting the optimum resistor”).
A manometer may be included in the circuit for training purposes to ensure an adequate pressure is generated (Fig 4). This T-piece connection is generally removed for patient prescription and use at home.
The mask should be positioned firmly over the nose and mouth, creating an effective seal.
Patient inspires with slightly larger than tidal volume breath through the mask.
Slightly active expiration is then performed through the PEP mask, maintaining a steady PEP of 10-20cmH20 through the middle of expiration.
This is repeated consecutively for a number of breaths, without losing the seal of the mask.
Cycles of tidal volume breaths are followed by the forced expiration technique, then coughing (if secretions are in the upper airways) to further mobilise secretions. The forced expiration technique is described in the ACBT and FET sections.
For an individual with unstable airways, FET may be performed into the mask, using the expiratory resistance to assist with stabilising the airways
(Lannefors 2009, Falk 1984, Groth 1985)
The patient should be given written instructions including the technique, prescription and cleaning of the device.
When using a mouthpiece PEP device, a nose-clip may be used in the initial phases of teaching the technique to minimise the loss of airflow through the nasal passages.
The mouthpiece should be positioned well into the mouth, with an effective seal created by the lips.
The resistance for PEP is selected according to the hole-size (PARI PEP) or on the dial (TheraPEP). Common hole-sizes often selected during the initial teaching session are 2.5 and 3.0 (see “Selecting the optimum resistor”).
A manometer may be included in the circuit for training purposes (for the PARI PEP devices) to ensure an adequate pressure is generated (Fig 5). In the PARI PEP, this connection is generally replaced by the non-manometer piece. The TheraPEP device has a manometer attached (Fig. 6).
Patient inspires with slightly larger than tidal volume breath through the mouthpiece.
Slightly active expiration is then performed through the mouthpiece, maintaining a steady PEP of 10-20cmH20 during mid-expiration.
This is repeated consecutively for a number of breaths, without losing the seal of the mouthpiece.
Cycles of tidal volume breaths are followed by FET, then coughing (if secretions are in the upper airways) to further mobilise secretions. FET is described in the ACBT and FET sections.


Physiology – PEP therapy is believed to temporarily increase functional residual capacity (FRC) and tidal volume. The positive pressure is thought to assist in splinting the airways open to reduce airway collapsibility and promote more homogenous expiratory airflow.
The adapted technique of huffing through the mask (a form of high pressure PEP) may further improve lung emptying and assist in moving the equal pressure point (EPP) to move more peripherally during expiration, avoiding airway collapse and further gas trapping.
Selecting the optimum resistor
The expiratory pressure is determined by:
Coloured resistor – mask PEP
Hole size – PARI PEP
Dial position – Therapep
To select the correct resistance, it is preferable to use a manometer in the circuit to enable an accurate assessment of expiratory pressures and provide feedback for the patient.
For most adults, a setting of 2.5 or 3.0 is appropriate for the initial teaching of the technique.
Once the patient has learnt the correct use of the device, the resistor size should be moved between 2.0, 2.5, 3.0 and 3.5 for several breaths each, resting between breaths as required. With each resistor size, note the achieved expiratory pressure and the length of flow. The ideal setting is the resistor size that provides expiratory pressures of 10-20cmH20 (maintained through the middle of expiration) with good expiratory flow and the least effort.
When the resistor size has been chosen, the patient should complete a full cycle of breaths to ascertain their ability to cope with this setting.
The expiratory pressure setting should be checked at every out-patient visit as their clinical status may have changed.
Patients should be given written instructions as to the assembly and care of the device and instructed not to alter the resistor setting.
For a simple, portable device a mouthpiece PEP can be set up by selecting the correct resistor as described above and placing it into a mouthpiece (Fig 7).

Prescription
PEP therapy may be performed in a seated or gravity assisted drainage position, depending on the optimal position for secretion clearance for each individual.
A typical cycle of PEP therapy consists of:
Breaths through the mask/mouthpiece – 6 to 12.
This will depend on the individual’s sputum volume, fatigue and dyspnoea levels.
Forced expiration technique, either outside of the mask/mouthpiece or through the mask (in the event of unstable/collapsible airways).
Cycles – 6 to 10
This will depend on the individual’s sputum volume, fatigue and dyspnoea levels.
The frequency of treatment will depend on the individuals’ symptoms and sputum volume, which will vary according to the clinical status. PEP therapy may be applied daily or twice daily in a stable clinical state. During an acute infection, the frequency, the number of breaths per cycle and the number of cycles may alter.
PEP therapy is an independent technique, able to be combined with other airway clearance options, including positioning and inhalation therapy and is beneficial for those patients with unstable or compliant airways.
The patient should be given written instructions including the technique, prescription and cleaning of the device.
There are clinical precautions which may influence the choice of this technique. It is therefore important that the technique is taught to the patient by a physiotherapist trained in this technique.
Clinical precautions for PEP therapy
Undrained pneumothorax or drained pneumothorax, due to risk of air leak
Post-lung lobectomy or lung transplantation, due to the risk of pneumothorax or compromise to the anastomosis
Haemodynamic instability or severe cardiovascular disease due to the application of positive pressure to the thorax, although with low pressure PEP, the risk is minimal compared to cough
Undrained empyema or lung abscess (due to the risk of sudden release of large volume of loculated fluid)
Active haemoptysis due to the risk of inducing excessive bleeding with the technique
Inability to tolerate due to increased work of breathing
Sinusitis
Facial fractures or surgery, particularly in the selection of a mask interface, if used
Middle ear infection, due to the risk of increased pressure within the Eustachian tubes during the technique
Clinical application and evidence for PEP therapy
Clinically, PEP therapy is applied in individuals with bronchiectasis. When applied in this population as well as in individuals with other suppurative lung disease with excess secretions, it has been found to be equally effective compared to conventional chest physiotherapy (GAD, manual techniques and coughing), autogenic drainage and slow expirations with glottis opened in lateral posture (ELTGOL) in secretion removal (Falk et al 1984) and improvement in cough-related quality of life when clinically stable and when experiencing an acute infection (Elkins 2006, Van Asperen 1987, Herrera-Cortina 2016).
It is important to include FET as part of PEP therapy to gain equivalent clearance of secretions compared to other techniques. The independence of the technique frequently appeals to individuals and for this reason it is often preferred over other ACTs.
For information on where to purchase the devices – see the Resources section.








