Background
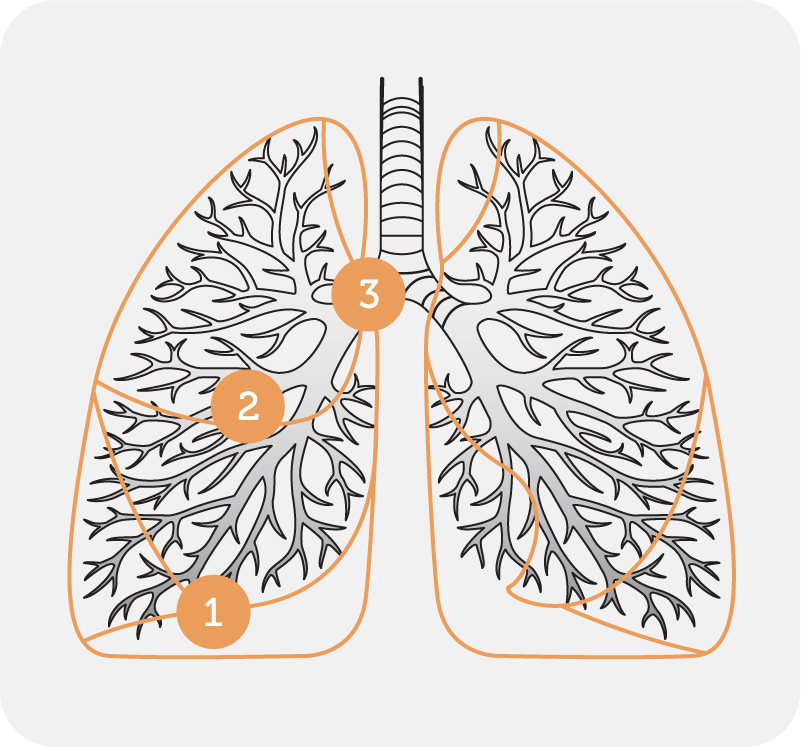
Autogenic drainage (AD) is an airway clearance technique which utilises controlled breathing at different lung volumes to loosen, mobilise and move secretions in three stages towards the larger central airways (Fig 1). The technique, developed by Jean Chevalier in Belgium in 1967, aims to maximise expiratory airflow, while avoiding dynamic airway collapse.
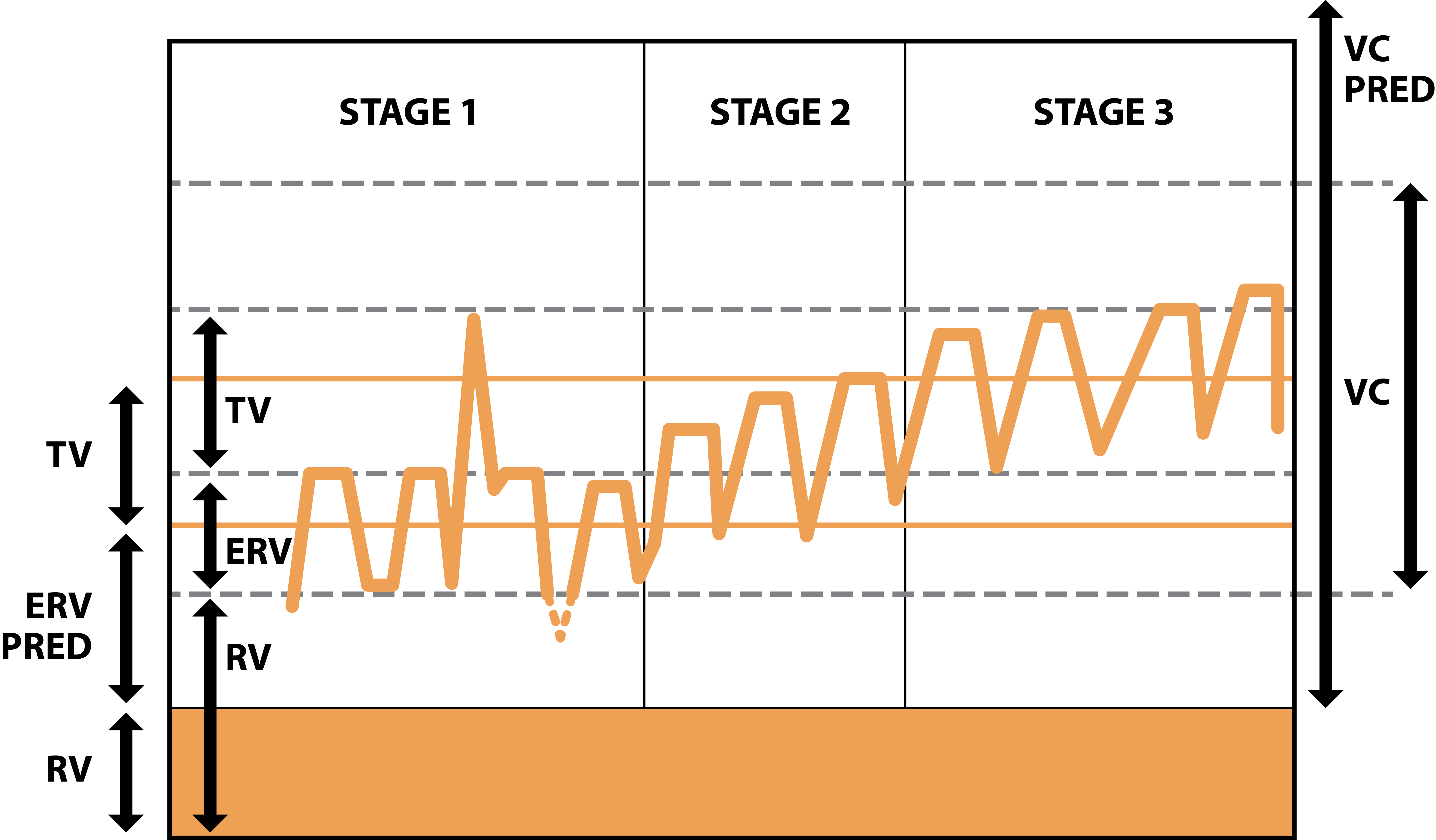
Stages of the technique (Fig. 2)
Stage 1 – low volume breaths to mobilise secretions from the peripheral airways
Stage 2 – medium (tidal) volume breaths to collect mucus from the middle airways
Stage 3 – large volume breaths enabling expectoration from central airways
How to perform the technique (Autogenic Drainage video)
Before commencing the technique, if the patient has symptoms of an upper airway blockage, it may be necessary to clear the upper airways by blowing the nose or, if necessary, using a nasal spray or sinus rinse. If prescribed, patients should take their bronchodilator medication. Nebulised mucolytics, such as normal saline or hypertonic saline, may be inhaled prior to or during this technique.
Position:
Sit in a well-supported position with a neutral lumbar spine and the neck and shoulders relaxed (Fig. 3)
Side lying, supine, prone
Breathing pattern (at different lung volumes):
Commence with a slow breath in through the nose, followed by a 2 to 3 second breath hold to facilitate collateral ventilation. Slow nasal breathing warms and humidifies the airways while reducing turbulent airflow. As the technique requires an open glottis, some patients may need to breathe in through their mouth, with or without the assistance of a piece of wide tubing (also used for huffing).
Exhale with the upper airways open (glottis and throat) down into respiratory reserve volume (via the nose is preferable but many patients prefer the mouth as it enhances the auditory feedback).
The expiratory force must be controlled in such a way that the expiratory airflow reaches the highest possible velocity without causing early airway compression. Patients with dynamic airway collapse may only need to breathe out with a relaxed sigh. Less advanced disease may need an expiration force which closely resembles a huff
Starting with low-volume breaths (Fig 2) from expiratory reserve volume, repeat breaths (inhalation and exhalation) until secretions are felt or heard gathering in the airways. Patients will need to use their abdominal muscles to expel the air at low lung volumes. This may take a number of breaths.
Once the sputum is heard (crackling) at low volume breaths, during the last part of each expiration, move to larger tidal volume breaths until the sputum is heard, or felt, to collect. This may also take a number of breaths.
Finally, after several larger (near vital capacity) breaths, the collected sputum reaches the upper airways where it can be cleared by a high volume huff and cough.
At all stages, the patient must be encouraged to suppress their cough until the sputum is in the central airways and ready to be easily expectorated
Prescription:
If prescribed, commence each session with bronchodilators
Nebulised mucolytics may be inhaled prior to or during the AD session
Nebulised antibiotics should be inhaled after the lungs have been cleared
The duration and number of the AD sessions depends on the total amount and the viscosity of the secretions
Patients with moderate to large quantities of sputum would benefit from at least two sessions a day
Experienced patients generally drain their lungs more quickly than others
Patients need to be encouraged to continue until the lungs are clear
The patient should be given written instructions including the technique and prescription.
Benefits of AD
No equipment is required
Patients can perform their airway clearance independently
Less effort is be required to expectorate which reduces stress on the pelvic floor
Disadvantages of AD
Patients generally need to be over 8 years old
The technique can be difficult to teach
Patients need the cognitive ability to understand the basic physiology behind the technique
To benefit from the auditory feedback, patients need to have a moderate or large amount of sputum
Evidence:
Published studies of autogenic drainage are limited with the majority of trials being in the cystic fibrosis (CF) cohort. The physiological rationale lends support for the use of AD in bronchiectasis. In a short term comparison of slow expirations with an open glottis, PEP therapy and AD, AD was found to be equally effective in sputum expectoration as slow expirations with an open glottis and improved quality of life (Herrero-Cortina 2016).
In a long term study of patients with CF comparing AD with postural drainage and percussion, the patients expressed a marked preference for AD (Davidson et al 1992).
In a comparison with ACBT, postural drainage and manual techniques, AD was found to be equally effective in improving lung function in patients with COPD with copious secretions (Savci 2000).
Greater expectoration was achieved with AD compared to PEP therapy (Lindemann 1990).
The long term effects of AD on quality of life and lung function, compared to other airway clearance techniques, was similar (Pryor 2010).
There are no studies evaluating assisted AD (AAD) in the bronchiectasis population group. In the Cystic fibrosis population, studies have found no provocation of GOR has been associated with AAD, bouncing or the combination of both (Van Ginderdeuren 2001, 2003).








