Modified Gravity Assisted Drainage and Positioning for Children
What is the technique?
Gravity assisted drainage (GAD) involves placing the patient in a position that allows gravity to assist the drainage of excess secretions from the airways to the point where they can be coughed or huffed out and expectorated.
As the awareness of gastro oesophageal reflux (GOR) in respiratory patients has increased, many centres are now advocating the use of modified drainage positions (ModGAD) for infants and children or those patients with suspected or demonstrated GOR. These modifications eliminate head down tip positions.
Different positions during play and activity are also used to alter airflow and optimize gas exchange, which can assist with secretion mobilization
How to perform the technique?
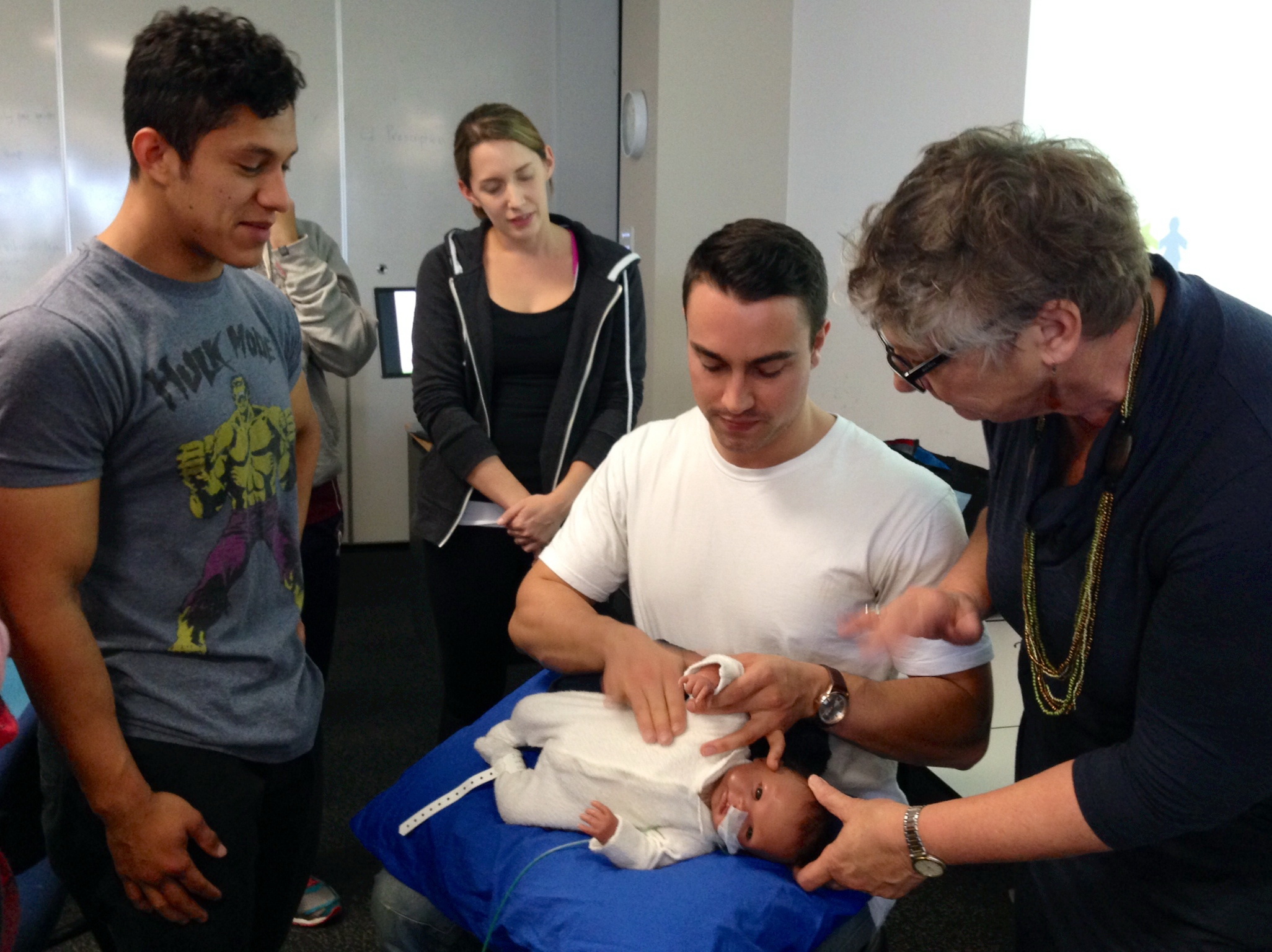
These positions may be achieved through placing toddlers on the care givers lap. Older children may often use a couch or bed.
Using a pillow on a therapy ball, grasped firmly between the therapist’s knees can provide a very versatile therapy surface, changing from bouncing and acceleration activities to positioning and manual techniques.
Each position may be held anywhere from 3 – 15 minutes
Prescription
Incorporate huffing or the active cycle of breathing technique (ACBT) when using ModGAD positions
The number of positions used and the time spent in each position will vary from person to person and depend on the clinical symptoms
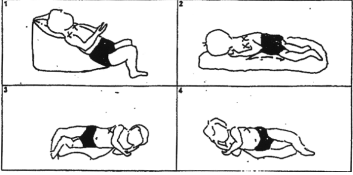
Modified gravity assisted drainage positons (Fig. 1)
Evidence for clinical application of ModGAD
ModGAD with the addition of manual techniques can be a useful airway clearance technique in children and adolescents provided the technique is tailored to the individual.
There is also evidence (both short and long-term) showing that the use of postural drainage with a head down tip in infants with cystic fibrosis, or those diagnosed with reflux, may actually increase the incidence of GOR (Button et al 1997a, 1997b, 1998, Malfroot et al 1991). A follow on from this study found that the ModGAD group had decreased respiratory complications compared to the GAD group (Button et al 2003).
There are also questions over the traditional taught practice of greater mucus clearance from the uppermost lung (as GAD assumes) or the dependent lung. The issue of debate is whether it is gravity or regional lung ventilation that has the greatest effect on airway clearance (Lannefors et al 1992). Most recent data has shown that in spontaneously breathing infants and children (up to the 2nd decade of life), the distribution of ventilation is more variable, rather than the previous teaching that children preferentially ventilate the non-dependent lung regions (Lupton-Smith et al 2014).








