Urinary incontinence in bronchiectasis
Urinary incontinence in non-CF bronchiectasis has been reported to affect between 47 to 55% of females with this condition (Rees 2013, Prys-Picard 2006) and is a more common problem compared to the general population.
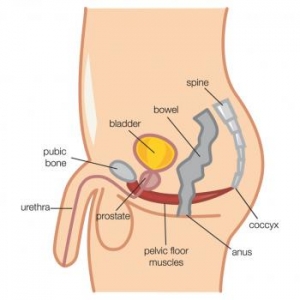
Symptoms of urinary incontinence may be present at least weekly and may have been experienced for several years (5-10 years). It is not known whether males with bronchiectasis suffer from symptoms of urinary incontinence, but it is an issue in men with other chronic lung conditions and may be a concern for men with bronchiectasis (Gumery 2002, Burge 2015).
Urinary incontinence has been linked to a poorer quality of life, the severity of which in females may be influenced by menopausal status and previous vaginal delivery in post-partum individuals (Vella 2009, Rees 2015).
Physiotherapy implications
- Do you have problems with leakage of urine in your pants during the day? (If yes, ask further questions to identify the type of incontinence)
- If you have problems with leakage, does it occur when you sneeze, cough, or lift heavy objects? (if yes, the patient may have symptoms of stress incontinence)
- If you have problems with leakage, is it associated with urgency symptoms or ‘busting to wee’? (if yes, the patient may have symptoms of urge incontinence)
- If you have problems with leakage, do you void less than 4 times per day, and tend to ‘hold on’ when you feel the need to void? (if yes, the patient may have incontinence due to voiding postponement)
Incontinence Impact questionnaire
The Questionnaire for female Urinary Incontinence Diagnosis – Bradley et al 2010
International Consultation on Incontinence-short form (ICIQ-SF) – Avery 2004
1.Teaching ‘The Knack’.
Coughing (including airway clearance therapy) or sneezing
Lifting weights or rising into standing from sitting
Stepping down heavily
How to do ‘The Knack’ Exercise?
Sit away from the back of the chair or stand tall with the chest lifted and the normal inward curve in the low back
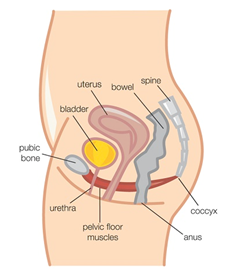
Lift and squeeze the muscles in and around all three pelvic openings (urethra, vagina and anus) immediately before a cough, sneeze or lift
Contract around all three pelvic openings at once, with a strong inward lift and squeeze of the pelvic floor muscles
Maintain this pelvic floor muscle contraction whilst doing a small cough
After a cough, relax the pelvic floor muscles back to normal resting level.
Progress this exercise with a more forceful cough, or repeating a couple of coughs in a row maintaining the pelvic floor contraction throughout.