Sinusitis and upper airway symptoms in bronchiectasis
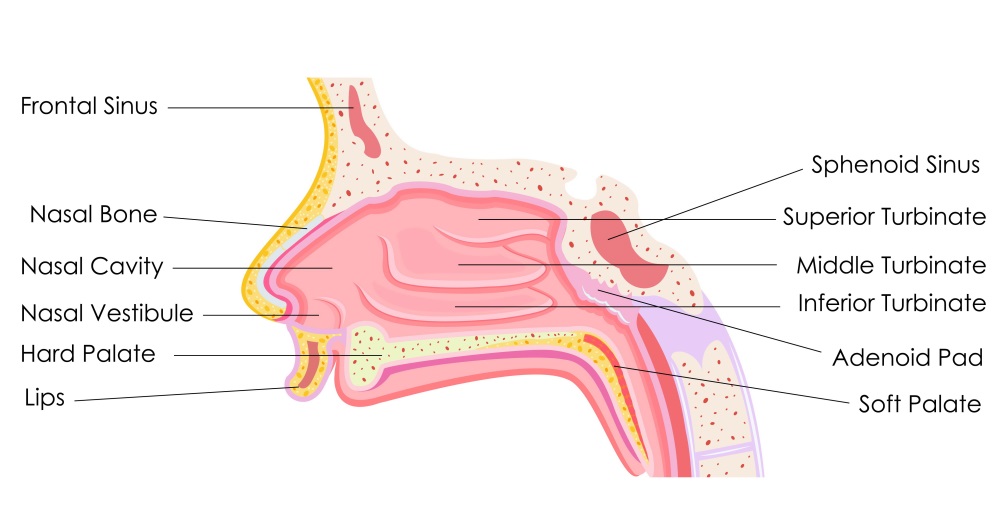
Upper airway symptoms in the form of rhinosinusitis (acute or chronic) may present in some people with bronchiectasis (Guilemany 2006, 2009a, 2009b). Rhinosinusitis is inflammation of the nasal passages and paranasal sinuses, which leads to a build-up of mucus production which may increase the risk of infection (Fig.1). If symptoms are present for more than 12 weeks, the condition is considered to be chronic (Benninger 2003).
Between 44% and 72% of people with bronchiectasis also have a diagnosis of rhinosinusitis. Rhinosinusitis is often linked to certain causes of bronchiectasis (Table 1) and may increase the risk of further chest infections, more severe bronchiectasis (Guilemany 2009a, 2009b, Yang 2017) and can have a negative effect on quality of life (Guilemany 2006).
Table 1. Rhinosinusitis and bronchiectasis
| Aetiology of bronchiectasis | Example of condition | Prevalence |
|---|---|---|
| Idiopathic | 45 – 84% | |
| Altered mucociliary clearance | Primary ciliary dyskinesia | Up to 100% |
| Immunodeficiency | Common variable immunodeficiency HIV | Up to 100% |
| Post-infective | Tuberculosis Mycobacterium avium complex Whooping cough Measles | 50% |
| Excess immune response | Allergic bronchopulmonary aspergillosis | 40-90% |
For people with bronchiectasis and chronic obstructive pulmonary disease, the prevalence of chronic rhinosinusitis is 58% and is linked to more severe bronichiectasis.
Common symptoms include:
nasal congestion/obstruction
nasal obstruction
face pain or pressure or fullness
itching and sneezing
altered sense of smell (hyposmia)
mucopurulent discharge
postnasal discharge
fever (acute only)
cough
Rhinosinusitis is diagnosed with nasal endoscopy and/or sinonasal CT scan. Endoscopy identifies the presence of secretions, oedema and polyps. HRCT scans of the sinuses identifies opacity in sinuses or changes in the mucosal layer. If symptoms are present for more than 12 weeks, the condition is considered chronic (Benninger 2003).
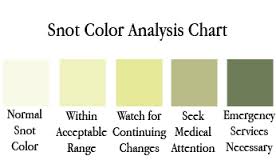
Patients should be encouraged to note the colour of their sinus secretions (Fig. 2)
Physiotherapy Implications
For people who report symptoms consistent with chronic rhinosinusitis or whose cause of bronchiectasis can be linked to upper airway symptoms, the physiotherapist should suspect the presence of chronic rhinosinusitis.
Assessment of symptoms can be measured by the following tools:
Nasal Symptom Questionnaire – This tool is identifying the presence or absence of 5 principal upper airway symptoms of rhinorrhea, post-nasal drip, decreased sense of smell, blocked nose and sneezing. A score of each symptom is summed with the total score ranging from 0 to 5. This is merely an identification of common symptoms. A score of 1-5 may be indicative of rhinosinusitis.
Sino-Nasal Outcome Test – This tool provides measures of 5 domains of sinus symptoms including rhinologic, extra-rhinologic, ear/facial, psychological and sleep symptoms. Scores range from 0 to 110. A higher score represent greater symptoms and a poorer quality of life and is likely to be indicative of rhinosinusitis (permission required for use).
Sinusitis outcomes questionnaire (Nathan et al 2004) – This tool identifies global symptoms as well as specific symptoms of the nose and sinuses, eyes, and chest. It also measures the economic burden of the disease. The severity of symptoms is assessed for a possible score ranging from 0 to 130. A higher score indicates that an individual is more symptomatic (permission required for use).
Total nasal symptom score (Downie et al 2004) – This tool assesses rhinitis symptoms of nasal obstruction, itching / sneezing and secretions, with a possible score ranging from 0 to 9. A higher score indicates an individual is more symptomatic (permission required for use).
Treatment options for chronic sinusitis
Medical therapies:
Saline irrigation
Topical corticosteroid nasal spray **
Systemic corticosteroids
Nonmacrolide antibiotic
Macrolide
Leukotriene pathway antagonist
H¹Antihistamine
Anti-IgE
Antibiotics (acute)
In severe cases, surgery may be required.
**Topical decongestants (Fig 4) can assist in relieving symptoms of blockage and facial pain.

Physiotherapy:
1. Nasal Irrigation / nasal lavage
A physiotherapist may recommend nasal irrigation to assist in the clearance of secretions. This may be a simple nasal spray using a saline spray (hypertonic or isotonic) or vigorous douching. Applications may be repeated several times per day to improve symptoms or before other topical treatments to improve exposure to the drug. A product frequently recommended by physicians is Sinus Rinse by Neil Med. Nasal irrigation can be an important part of the management of sino-nasal conditions. Patients must be instructed to clean the device daily as per the manufacturers instructions. Further research is required to ascertain the tonicity and use of additives to the solution.
An effective treatment strategy to assist with the clearance of excess secretions in the sinus region may be nebulised saline (0.9%) or hypertonic saline (3-6%) via a nebuliser.
This can be achieved with a mask nebuliser or the Pari Sinus nebuliser (Fig 5).

3. Ultrasound
Physiotherapists may apply therapeutic pulsed ultrasound therapy (Young 2010, Hosoein 2010, Ansari 2012).
This may be applied over the sinuses at a therapeutic ultrasound level (1.0 W/cm2 in continuous mode) for approximately 10 minutes each day, with the transducer moved in small circular motions over both sides of the nose and forehead (over the sinuses) (Fig 3).









