Musculoskeletal issues
Specific musculoskeletal complications may be present in those with bronchiectasis.
In those diagnosed with rheumatoid arthritis, bronchiectasis may be a respiratory consequence (Shadick 1994). Pain experienced in individuals whose lung condition is related to this cause may be a direct reflection of the symptoms of rheumatoid arthritis, which may affect multiple joints.
Other possible sources of pain are co-existing musculoskeletal conditions. According to dual energy x-ray absorptiometry (DEXA) scans, osteopaenia may affect between 30% to 55% of adults with bronchiectasis, while osteoporosis may be present in 14% to 25% (Dave 2009, Baris 2011). In children, the prevalence of osteopaenia is 27% to 37% and osteoporosis is 16% to 41% (Guran 2008).
Risk factors for reduced bone mineral density are:
previous use of corticosteroids
increasing age
nutritional deficiency (low body mass index and fat free mass index)
postmenopausal status
reduced activity
Complications of osteoporosis may include rib fractures or vertebral crush fractures.
Peripheral skeletal muscle complications have been reported, with reduced muscle strength and endurance (Gale 2012). Increased levels of fatigue are also common. These changes may present as symptoms of peripheral muscle pain or tightness accompanied by fatigue (Ozalp 2012).
In older patients, another common musculoskeletal condition may be osteoarthritis, which may also present with joint pain and stiffness.
Chest wall pain may be due to respiratory muscle fatigue or overuse and may affect both children and adults (King 2012). It may be triggered by coughing or airway clearance therapy. For this reason, this symptom may intensify during an acute exacerbation of bronchiectasis.
Physiotherapy implications
As part of a standard assessment, a physiotherapist should ask about the presence of pain.
This is particularly important for any patient with a history of:
rheumatoid arthritis
osteoporosis
osteopaenia
osteoarthritis
Assessment should include:
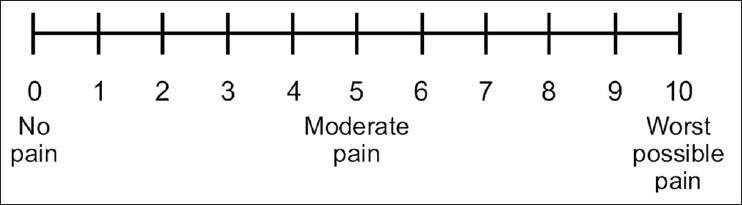
pain intensity, with the option of using a visual analogue scale (Fig. 1) or numerical rating scale (Fig. 2)
location of the pain using a body chart (Fig. 3)
pain behaviour over 24 hour period
aggravating and easing pain factors, including the impact of recommended physiotherapy routines
physical assessment as appropriate
No pain Worst possible pain
I________________________________________________________________I
Other tools which provide further details regarding the impact of pain are available, include:
Brief Pain Inventory-short form (Cleeland 1994)
McGill Pain Questionnaire-short form (Melzack 1975)
The negative implications of musculoskeletal conditions can include:
an inability to exercise at an appropriate intensity
an inability to perform airway clearance routines
a reduction in movement of the thoracic rib cage resulting in decreased lung function and an increased risk of exacerbations
Treatment options
In the case of pain aggravating physiotherapy treatment, such as airway clearance or exercise or contributing to a poorer quality of life, suggestions to modify the exercise routine or airway clearance techniques may be necessary.
This could include:
modification of positioning
modification of frequency of the prescribed routine
supportive techniques to minimise discomfort during techniques, such as coughing
modification of exercise intensity
alteration of exercise modality or routine
These changes can be monitored and reviewed on a regular basis.
Assessment findings from the physical evaluation may indicate the need for the following treatment:
exercise prescription
mobilisation and manual therapy techniques
recommendations for postural modifications
This treatment should be provided by experienced health professionals trained in these techniques with this patient group.








